To BB or Not To BB (Glow)? This article is in response to the many emails I have received requesting guidance on a new treatment taking the world by storm: “BB GLOW”.
BB Glow entails using a Microneedling device to tattoo BB Cream into the skin as a form of semi-permanent makeup to “hide blemishes and allow one to wake up looking radiant”. (For the purpose of this discussion, while “BB Cream” is a marketing term used generically, I am referring to special ampoules of solutions that are sold for use with Microneedling and NOT the “BB Cream” from the local beauty store.)
My first reaction to this was, “why are we even talking about this?” It seems vanity and insanity know no bounds. Instinctively, most of the enquirers suspect this is a bad idea, and, given the enthusiasm within the media from consumers and practitioners alike, the desire is now to counter this apparent wild abandonment with specific scientific data.
Disturbing the Balance of Nature
The skin barrier has a physical, chemical, and immunological component. Disturb any of these complex components and the outcome may be problematic. Disturb all three simultaneously and the risk of an adverse outcome skyrockets.
Microneedling breaches the physical barrier by creating temporary channels that facilitate infusion of topically applied substances. These ingredients interact with the chemical component of the skin, influencing change for good (or bad) via signalling systems. Immunological reactions are mounted in response to environmental challenges (foreign material) via the innate and adaptive immune systems. The former tends to be a poorly discriminating, rapid response without memory, while the latter is highly specific in response to previous exposure (memory) over time. [Cells implicated in the innate response include phagocytes, eosinophils, mast cells, NK cells and keratinocytes. Cells implicated in the adaptive response include dendritic cells, Langerhans cells and lymphocytes (B cells and T cells).[1] ]
The Disruptors
Microneedling has been around for a while and is known to be relatively safe compared with other treatment modalities. Why, then, are the risks higher with Microneedling (tattooing) BB Cream as opposed to any other cream used with a cosmetic device for home treatments?
[As a side note: This gets a bit confusing on multiple levels due to definitions and differing recommendations within the industry. See following definitions:
- Cosmetic Needling: Industry classification of microneedling is according to needle length. Less than 0.5 mm is considered “Cosmetic”, and therefore safe to use at home to infuse appropriate topical ingredients to support and maximize cell function.
- Medical Needling: Many companies encourage infusion of products after “Medical” needling, using needle depths exceeding 0.5 mm “in-clinic”. This practice has more to do with “upselling”, and benefits the suppliers rather than the patient. Improvements to the patient following one application of a product on a monthly basis are minimal compared to the risks of systemic infiltration of (mostly non-tested) ingredients. These include allergic reactions, post-inflammatory hyperpigmentation (PIH), scarring, and granulomas. Fortunately, these complications are less prevalent when compared to other treatments in the industry, but they are not insignificant and they are avoidable for the most part. In view of this, I recommend “cosmetic” or home “infusion” of the appropriate ingredients instead of “in-clinic”, as daily application has a far greater benefit with less risk of an immune response. (Consider going to the gym daily with low intensity, vs. once a month with high intensity. Also note that any topical substance may cause an immune response with an adverse outcome, even if confined to the epidermis. One needs to consider the risk/benefit ratio. The greater the number of ingredients in a cosmetic topical product, the greater the risk.)
The above definitions clearly show that when one has an “in-clinic” microneedling treatment, it is considered Medical, and involves a needle length of 0.5 mm or more. Here is where the confusion arises. BB Glow advocates are instead recommending an “in-clinic” treatment that is considered Cosmetic, using needle lengths of less than o.5 mm. They do this because they mistakenly believe that confining ingredients to the epidermis renders this treatment safe.]
Permanent Make-Up is also widely used with relative safety, leaving pigment implanted in the skin. How is BB Glow any different?
The difference between creams infused for antiaging versus BB Cream has everything to do with the type and number of ingredients. With Microneedling alone, the mechanical effects on the skin are of very short duration. With antiaging creams, ingredients absorbed through the channels are mostly biodegradable, or are diluted, carried away, and excreted, so their chemical effects are limited. In contrast, non-degradable substances in BB Cream accumulate over time and trigger an immune response which may end up being prolonged. The quantity of non-degradable material deposited over an entire face (every few months) is also significantly more than, for example, brows or eye liner. Furthermore, the number of ingredients used for brows or lips tends to be in the single digits, as opposed to 40-plus ingredients in some BB Creams.
How Do We Know When We Are Doing Harm?
As practitioners, we have a professional duty and responsibility to “First Do No Harm”. Sometimes the answer is a ‘no brainer’ when we infuse something that causes an allergic reaction or contact dermatitis. The greater challenge is when the adverse outcome is delayed or invisible to the naked eye. In some cases it may take years to show, e.g. cancer. It is especially tempting to throw caution to the wind when “instant gratification” is involved. If it looks great, why not? Enter BB Cream Microneedling treatments or semi-permanent foundation, also known as BB Glow or MesoBB.
What Is Semi-Permanent BB Cream? What Prompted This Idea?
The art of permanent makeup has also been around for a while. The upside is always looking your best with little to no effort, and the downside is an irreversible blemish. Two areas, eye-liner and lips, were initially most popular, but now brows are all the rage. Microblading, in the right hands, enables depositing pigment in super fine lines, thus creating the impression of a real hair. The natural progression of this thought process is, “if it is ok to put pigment into the lips or the brows, why not the entire face?”
The advent of microneedling devices has facilitated the ease of performing BB Glow treatments. BB Cream became popular due to the appeal of “having it all” in one tube. Variations include primer, foundation, concealer, moisturizer, skin treatment, and SPF all-in-one. Given the popularity of Microneedling and BB Cream, it did not take long for someone to try combining the two and “tattooing” the pigment into the skin. A mask is frequently applied after the treatment to enhance absorption of the ingredients. Needling protocols vary, using depths from 0.1 to 1 mm, and results are quoted as lasting from weeks to years. “Before” and “after” pictures can be remarkable. Hence, the end justifies the means and we now have a runaway train on our hands.
What Are the Benefits of BB Glow?
The allure in this case is waking up all year round with a naturally glowing, smooth complexion without having to apply foundation. Immediate benefits are touted as saving time and money. No more smudges or need for touch-up after a rough day in the world. An added benefit from the microneedling aspect is collagen induction to smooth out wrinkles and tighten pores. (I probably had you at “naturally glowing, smooth complexion”.)
Are There Marketing Red Flags?
After reading about some of the benefits on websites and in beauty magazines, a few points caught my eye. “EGF” (Epidermal Growth Factor) randomly thrown into the mix of the ingredient stack in some products makes no sense. That is a huge can of worms all on its own, and you can read further here. Statements like, “100% safe and natural ingredients”, and, “it’s so new that it is not yet approved by the FDA”, are automatic red flags.
What Are the Risks of BB Glow?
Many things are possible, but not all things are prudent. As with most things that are bad for us, we end up sacrificing “the permanent on the altar of the temporary”. It may look good and feel good now, but we will pay a high price later. Most of the risks of BB Glow are related to the ingredients infused. These may include (but are not limited to) allergic reactions, contact dermatitis, infection, PIH, granulomas, scarring, organ toxicity, cell damage, and cancer.
As a point of reference, here is a list of some of the ingredients found in BB Cream:
Water, Glycerin, Niacinamide, Propylene Glycol, Mineral Oil, Ethanol, Titanium Dioxide(CI 77891), Aluminum Hydroxide, Triethoxycaprylylsilane, Caprylic/Capric Triglyceride, Cyclohexasiloxan, Cetyl Ethylhexanoate, Talc, Magnesium Aluminum Silicate, Polysorbate 80, Micro Crystaline Wax, Cetostearyl Alcohol, Stearic Acid, Glyceryl Stearate(se), Chlorphenesin, Dimethicone, Sorbitan Sesquioleate, Yellow Oxide Of Iron (CI 77492), Beeswax, Methyl Paraben, Fragrance, Disodium EDTA, Allantoin, Xanthan Gum, Red Oxide of Iron (CI 77491), Sodium PCA, Aloe Barbadensis Leaf Extract, Persea Gratissima (Avocado) Fruit Extract, PEG-60 Hydrogenated Castor Oil Tocopheryl Acetate, EGF, Propyl Paraben, Phenoxyethanol.
(Keep in mind that virtually all safety studies on cosmetic ingredients are confined to application on intact skin. They are also done in the context of a specific isolated ingredient, and evidence of safety is not necessarily applicable when combined with other ingredients due to interactions. There are no safety studies pertaining to “injecting” a concoction like the above into the body because it is an insane thing to do for one, and impossible to cover all the variables when so many ingredients are included.)
- Allergic Reactions
You may recall the uproar years ago when “nanotechnology” was introduced into the cosmetic field. It was feared that by miniaturizing molecules, they would enter the body in larger quantities. Nano-elements behave differently to their presence in bulk. We know little of how quantum mechanics influence substances of nanoscale and how they may behave inside the body. These molecules are charged, which is one mechanism facilitating surface reactivity with the surrounding tissue. Non-degradable, or slowly degradable particles, may accumulate over time within organs with potential for toxicity.[2][3] All of this previous uproar was in the context of “intact skin”, and yet here we are decades later breaking down the skin barrier with needling devices to permanently or semi-permanently implant foreign material into the largest organ of the body.
Reassurances: “But we are averting risk by only working in the epidermis.”
Practitioners quoted in articles espousing this treatment discuss using a needle depth that “stops short of the dermis”, yet in their accompanying pictures, pin-point bleeding is sometimes visible. (Denotes evidence of dermal penetration.) Can any practitioner guarantee they are only working in the epidermis? Some say, “Yes! One can be certain if nano-needles are used which treat only the upper layers of the epidermis.” However, this is a moot point. They mistakenly believe that by restricting deposition of material into the epidermis alone, the risks of an immune response are minimized. While less absorption will occur using this technique (which means results will be very short-lived), allergic reactions are not necessarily “dose-dependent”, nor does it depend on the allergen (foreign material) entering the dermis. There are many mechanisms that facilitate allergic reactions. One way is via cells that migrate into the epidermis (Langerhans cells) to “capture” foreign substances and drag them back into the dermis and into the lymph nodes. This migration of Langerhans cells depends on epidermal cytokines, e.g. TNF-α and IL-1β.[4]
Consider this for a moment. One of the tests used to determine allergies is called a “scratch test”. A small scratch is created in the epidermis and common allergy-provoking substances are applied to this tiny area. After 20 minutes the skin is examined for a reaction in the form of redness, swelling, or a rash. One of the BB formulas sent to me for my opinion contained 44 ingredients. Forty-four! Not only that, but it is to be applied over a LARGE area. Whether it is BB Cream you are applying after Microneedling, or any other substance, remember in essence that you are doing a giant allergy test. The higher the ingredient count, the higher the risk.
Ingredients in BB Cream most likely associated with allergic reactions: While any ingredient may be associated with allergy, the most likely are fragrance, methyl paraben, propyl paraben, mineral oil, sorbitan sesquioleate and phenoxyethanol.
- Contact Dermatitis
With irritant contact dermatitis, a certain minimum (dose) exposure to a substance is needed, whereas with allergic contact dermatitis (ACD), tiny quantities of allergens are sufficient to trigger a response. While symptoms may be similar, the underlying mechanisms differ. “Irritant contact dermatitis (ICD), evolves as a consequence of direct toxic effects of physical or chemical agents resulting in keratinocyte damage and local inflammation, while ACD critically depends on adaptive immunity.”[5]
Logically, underlying causes include anything that facilitates increased absorption of foreign material into the skin. Impaired barrier defense results with friction, over-exposure to water, chemicals (acids, alkalis, emulsifiers, detergents and solvents), and, of course, Microneedling (cosmetic and medical). Thus, allergic and irritant contact dermatitis may co-exist, especially in the context of Microneedling, both cosmetic and medical.
Ingredients most likely associated with contact dermatitis: Fragrance, methyl paraben, propyl paraben, propylene glycol, sorbitan sesquioleate, and phenoxyethanol. Ingredients associated with depletion of bilayers include emulsifiers like cetostearyl alcohol, stearic acid, glyceryl stearate, polysorbate 80, and sorbitan sesquioleate.
- Post-Inflammatory Hyperpigmentation
Post-inflammatory hyperpigmentation (PIH) is perhaps the most commonly reported serious side effect with microneedling. A common denominator in most cases is Microneedling PLUS something that amplified the inflammatory cascade. There is nothing like a foreign body reaction to get inflammation going. Try a sliver in your finger for a week. The risk for PIH increases in higher Fitzpatrick skin types. Sadly, the group at highest risk of harm are the target market for BB Glow treatment. They are more prone to hyperpigmentation and uneven skin tone after sun exposure or acne, as examples. (The treatment seems to have originated in Korea, and Asian skins are often associated with acne.)
Ingredients most likely associated with PIH: Fragrance, methyl paraben, propyl paraben propylene glycol, sorbitan sesquioleate, and phenoxyethanol.
- Infections
I would hope that all practitioners employ appropriate bloodborne pathogen prevention practices to avoid cross-contamination. Hep B/C and HIV ought not to be a factor. However, secondary infection after Microneedling, although rare, is a possibility. Let’s not create the ideal environment to change this statistic. If we look at the literature for infections related to “implants”, which includes dermal fillers, the introduction of material into the body raises the risk of infection considerably, even when adequate precautions of pre-surgical skin cleansing have occurred.[6] In these studies, the implants were sterile (as opposed to BB Cream ampoules filled with preservatives). Why is this the case if the implant is sterile and the skin is cleaned? The answer seems to be due to a phenomenon called “biofilms”. Pathogenic bacteria (those that are harmful) can clump together and also stick to things (like foreign material) and become covered in a “film” that protects them from being detected by immune cells or antibiotics that would normally destroy them. Staphylococcus aureus biofilm is a common offender.
Interestingly, when it came to fillers in this particular study, infection was greater with lesser depths (1 mm vs. 3 mm). Clinically visible infections with dermal fillers are rare in healthy individuals, but as high as 19% in patients with HIV, cancer, or diabetes[7][8][9]. Infections were more common, though perhaps delayed in onset, when minimally biodegradable fillers were used.[10] (The take-home lesson is that tattooing foreign material into the skin affords “bad surface bacteria” an opportunity to enter and set up home on the “building blocks” you have laid down for them.)
- Granulomas
Granulomas are a type of scar where the body tries to “wall off” foreign material that it is unable to eliminate. Fortunately, granulomas caused by Microneedling alone are not that common, but the incidence is increasing as distributors promote topical products to apply during and after treatment with the express purpose of infusion. Some of these patients present with systemic illness, some having required hospitalization for intravenous antibiotics, steroids, and immunosuppressive drugs. Presenting symptoms may include rash (erythematous papules coalescing into plaques), fever, arthralgia, and erythema nodosum.
Ingredients most likely associated with Granulomas: Titanium dioxide [11], dimethicone [12], Talc[13], iron oxide [I11], aluminum hydroxide [14] and triethoxycaprylylsilane.
- Scarring
Microneedling a patient with keloid has the potential to make things worse. However, the scarring I am referring to here is different in that it may not be visible to the naked eye, but the fibrous tissue that results will reduce pliability of the skin. Scarring is directly proportionate to the inflammatory cascade of any wound healing process. Thus, where foreign material is implanted, we can expect a chronic, low grade inflammatory response which would lead to scar collagen over time.
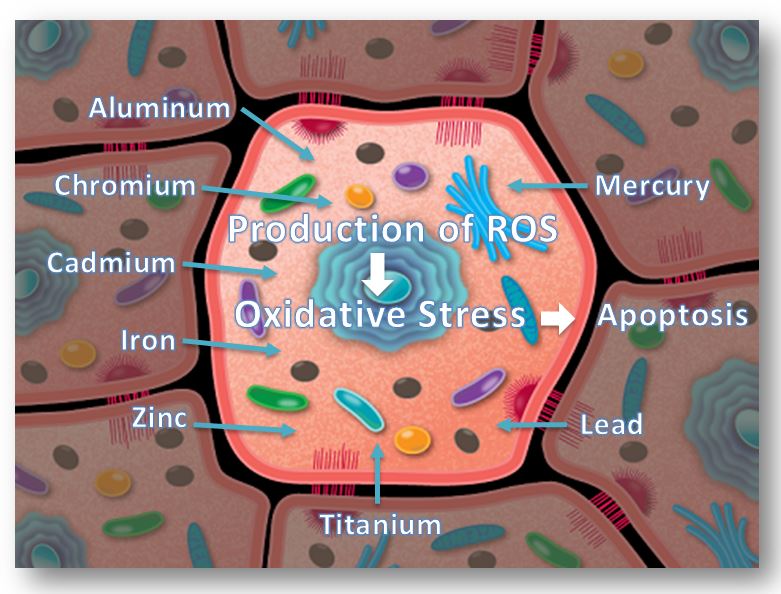
- Cell Damage and Cancer
Particles that are deposited into the body, particularly metals, initiate oxidative stress, inducing redox-sensitive transcription factors associated with inflammation. The skin’s susceptibility to UV radiation is well documented, and the combined effect of UVB and nanoparticles co-exposure is more significant than we realize. What are the possible effects of metals on keratinocytes? – DNA damage and cell death.[15][16][17]
This is a vast topic which would overshadow the intention of this article, but just as a reminder, it is not only about environmental interactions with ingredients imbedded in the skin, but also how molecules may interact with each other. For instance, “titanium dioxide” may cause bioaccumulation of copper (perhaps used in a topical cream on a daily basis after a BB Glow treatment) to the point of toxicity.[18]
Ingredients most likely associated with cell damage and cancer: Titanium dioxide, cyclohexasiloxan, mineral oil, iron oxide [IOG], aluminum hydroxide [AG], Aloe Barbadensis Leaf Extract.
- MRI (Magnetic Resonance Imaging)
You may recall from your childhood days the intrigue of moving a magnet beneath paper covered in iron filings. Any metal with magnetic properties will be disturbed by an MRI. Iron Oxide in particular may cause burns due to the magnetic field moving electrons to create a current that heats the skin. The image may also contain a black spot due to the pigment, thus obscuring the structures from view beneath it.[19]
- Q-Switch Laser: As a side note, white inks containing iron oxides and titanium dioxide may turn irreversibly black after QS laser irradiation.[20] In addition, standard universal precautions in the use of IPL and lasers for treatments other than tattoo removal need to be adhered to in patients with pre-existing (BB) tattoos to avoid burns.
In Summary
On the one hand, we have cosmetic Microneedling with the infusion of biodegradable (preferably native) material for home care. On the other hand, we have “in-clinic” cosmetic (or medical) Microneedling with the infusion/tattooing of BB Cream. Why is one OK and not the other? As you can see, it is not the needle depth that differentiates the two — it is mainly the non-degradable ingredients and the immune response that they cause. This response may be delayed and/or prolonged. The associated inflammation leads to complications, such as scarring, granulomas, PIH, organ toxicity, cellular damage, and even cancer. Non-degradable substances also provide a habitat for biofilms that are associated with antibiotic resistance and chronic infection. The vast quantity of ingredients, (40-plus in BB Cream), increases the risk of allergies and contact dermatitis, as well as the large surface area being treated when compared to permanent makeup of lips and brows. Risk is not averted by simply confining the ingredients to the epidermis. Given all the above, and in the absence of safety studies, the risks clearly outweigh the benefits.
For further reading, see The Concise Guide to Dermal Needling, Third Medical Edition – Revised & Expanded, pages 94-107. (Ingredients to avoid with Dermal Needling.)
©2005 – 2020, Dr. Lance Setterfield. All Rights Reserved. Needling Guide™ and the Needling Guide Logo are trademarks of Dr. Lance Setterfield. All other product names and trademarks are property of their respective owners, and are used for identification purposes only. Communications between the user and NeedlingGuide.com are protected by our Privacy Policy. NeedlingGuide.com provides access to this site, and the content herein, subject to Terms of Service. Your access to the website is subject to such Terms of Service. Use of this website is at your own risk. All content, including any information, charts, documents, audio/video, products, software, and services is provided ‘as is’ with no warranties or guarantees whatsoever.
References:
[1] Christine Bangert MD, Patrick M. Brunner MD, Georg Stingl MD. Immune functions of the skin. Clinics in Dermatology, Volume 29, Issue 4, July–August 2011, Pages 360-376. https://www.sciencedirect.com/science/article/pii/S0738081X11000320?via%3Dihub
[2] Eudald Casals, Socorro Vázquez-Campos, Neus G. Bastús, Victor Puntes. TrAC Distribution and potential toxicity of engineered inorganic nanoparticles and carbon nanostructures in biological systems. Trends in Analytical Chemistry, Volume 27, Issue 8, September 2008, Pages 672-683. https://www.sciencedirect.com/science/article/abs/pii/S0165993608001428
[3] Stephan T. Stern, Scott E. McNeil; Nanotechnology Safety Concerns Revisited, Toxicological Sciences, Volume 101, Issue 1, 1 January 2008, Pages 4–21, https://doi.org/10.1093/toxsci/kfm169
[4] Ian Kimber, Rebecca J Dehttp://web.archive.org/web/20201212214630/https://doi.org/10.1093/toxsci/kfm169arman, Marie Cumberbatch, Russell JD Huby. Langerhans cells and chemical allergy. Current Opinion in Immunology, Volume 10, Issue 6, 1998, Pages 614-619, ISSN 0952-7915, https://doi.org/10.1016/S0952-7915(98)80078-2
[5] Martin, S. F., Esser, P. R., Weber, F. C., Jakob, T., Freudenberg, M. A., Schmidt, M. and Goebeler, M. (2011), Mechanisms of chemical-induced innate immunity in allergic contact dermatitis. Allergy, 66: 1152–1163. doi:10.1111/j.1398-9995.2011.02652.x http://onlinelibrary.wiley.com/doi/10.1111/j.1398-9995.2011.02652.x/full, https://www.ncbi.nlm.nih.gov/pubmed/21599706
[6] Yi Wang, Valery Leng, Viraj Patel & K. Scott Phillips. Injections through skin colonized with Staphylococcus aureus biofilm introduce contamination despite standard antimicrobial preparation procedures. Scientific Reports volume 7, Article number: 45070 (2017) https://www.nature.com/articles/srep45070
[7] Keefe, J., Wauk, L., Chu, S. & DeLustro, F. Collagen biomaterialsClinical use of injectable bovine collagen: A decade of experience. Clin. Mater. 9, 155–162 (1992) https://www.ncbi.nlm.nih.gov/pubmed/10171198?dopt=Abstract&holding=npg
[8] Lowe, N. J., Maxwell, C. A. & Patnaik, R. Adverse reactions to dermal fillers: review. Dermatol. Surg. Off. Publ. Am. Soc. Dermatol. Surg. Al 31, 1616–1625 (2005). https://pubmed.ncbi.nlm.nih.gov/16416647/
[9] Nadarajah, J. T. et al. Infectious Complications of Bio-Alcamid Filler Used for HIV-Related Facial Lipoatrophy. Clin. Infect. Dis. 55, 1568–1574 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22942210?dopt=Abstract&holding=npg
[10] Funt, D. & Pavicic, T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin. Cosmet. Investig. Dermatol. 6, 295–316 (2013). https://www.ncbi.nlm.nih.gov/pubmed/24363560?dopt=Abstract&holding=npg
[11] Jones, B. , Oh, C. and Egan, C. A. (2008), Spontaneous resolution of a delayed granulomatous reaction to cosmetic tattoo. International Journal of Dermatology, 47: 59-60. doi:10.1111/j.1365-4632.2007.03386.x
[12] Giuseppe Ficarra, Adalberto Mosqueda-Taylor, Roman Carlos, Silicone granuloma of the facial tissues: A report of seven cases, Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, Volume 94, Issue 1, 2002, Pages 65-73, ISSN 1079-2104, https://doi.org/10.1067/moe.2002.124459
[13] What causes foreign body granulomas? … Talc. https://dermnetnz.org/topics/foreign-body-granuloma
[14] Erdohazi M, Newman RL. Aluminium hydroxide granuloma. Br Med J. 1971;3(5775):621-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1798739/
[15] Murray, A.R., Kisin, E., Inman, A. et al. Oxidative Stress and Dermal Toxicity of Iron Oxide Nanoparticles In Vitro. Cell Biochem Biophys (2013) 67: 461. https://doi.org/10.1007/s12013-012-9367-9
[16] Shukla, Ritesh K.; Kumar, Ashutosh; Pandey, Alok K.; Singh, Shashi S.; Dhawan, Alok. Titanium Dioxide Nanoparticles Induce Oxidative Stress-Mediated Apoptosis in Human Keratinocyte Cells. Journal of Biomedical Nanotechnology, Volume 7, Number 1, January 2011, pp. 100-101(2) American Scientific Publishers. DOI: https://doi.org/10.1166/jbn.2011.1221
[17] Ryu, WI., Park, YH., Bae, H.C. et al. ZnO nanoparticle induces apoptosis by ROS triggered mitochondrial pathway in human keratinocytes. Mol. Cell. Toxicol. (2014) 10: 387. https://doi.org/10.1007/s13273-014-0043-6
[18] Liu K, Lin X, Zhao J. Toxic effects of the interaction of titanium dioxide nanoparticles with chemicals or physical factors. Int J Nanomedicine. 2013;8:2509-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3720578/
[19] Ross JR, Matava MJ. Tattoo-induced skin “burn” during magnetic resonance imaging in a professional football player: a case report. Sports Health. 2011;3(5):431-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445217/
[20] Ortiz, A. E. and Alster, T. S. (2012), Rising Concern over Cosmetic Tattoos. https://pubmed.ncbi.nlm.nih.gov/22093105/